3 Easy-To-Use Design Tools for Understanding Patient Needs
More and more, we recognize the need to engage patients in healthcare. “Improving patient engagement” is becoming a popular theme in hospital strategic plans, and governments are pushing for it to become a bigger priority too.
So, we get that we have to engage patients more, but how do we do that? We don’t want to just engage for the sake of engaging, right?
Here are 3 free and easy-to-use tools for engaging with patients that will give you the insights you need to make their experience better.
1. A FEEDBACK GRID
A feedback grid is a quick and constructive way to gather feedback from patients about a specific program or service, their overall experience, or whatever else you may be looking to improve.
It’s a very adaptable activity—you can do it in a group setting, for example, if you’re running a regular program, or you can do it with individuals. Allow 10-15 minutes. You’ll need a two-by-two grid that fills the page, with the following labelled quadrants:
Upper left—“What I like about this idea”
Upper right—“What I would improve”
Lower left—“What questions I still have”
Lower right—“What new ideas does this give me”
Or download Overlap’s free feedback grid:
Give the patient(s) 10 minutes to jot down their notes in the appropriate quadrants.
Optional: If you ask folks to use sticky notes instead of writing directly on the feedback grid, you can cluster the feedback later to spot themes that suggest criteria for evaluating this and other ideas.
2. An Empathy Map
An empathy map gives you a more holistic understanding of your patient’s experience, as well as their needs and obstacles.
Learn more about empathy maps here.
Again, you can do this activity with individuals or in a group. If you’re asking an individual, we suggest taking them through the map orally—treating it like a conversation can take some of the pressure off of the patient, and it helps build a connection with them.
If you’re working in a group, each person can fill out their own empathy map. Alternatively, you can also facilitate the group so that each member contributes to one large empathy map.
Tip: tailor your questions to the subject you’re exploring. Is it the space? Is it the whole service experience? Is it the experience in the waiting room? Is it their experience on a waitlist?
What are some things you see in our space?
What are some things you hear in our space?
What are some things you say in our space?
What are some things you think in our space?
What are some things you are doing in our space?
What are some things you are feeling in our space?
What are some things you are trying to get done in our space?
What gets in the way of you getting those things done?
What single change could we make that would make the biggest impact?
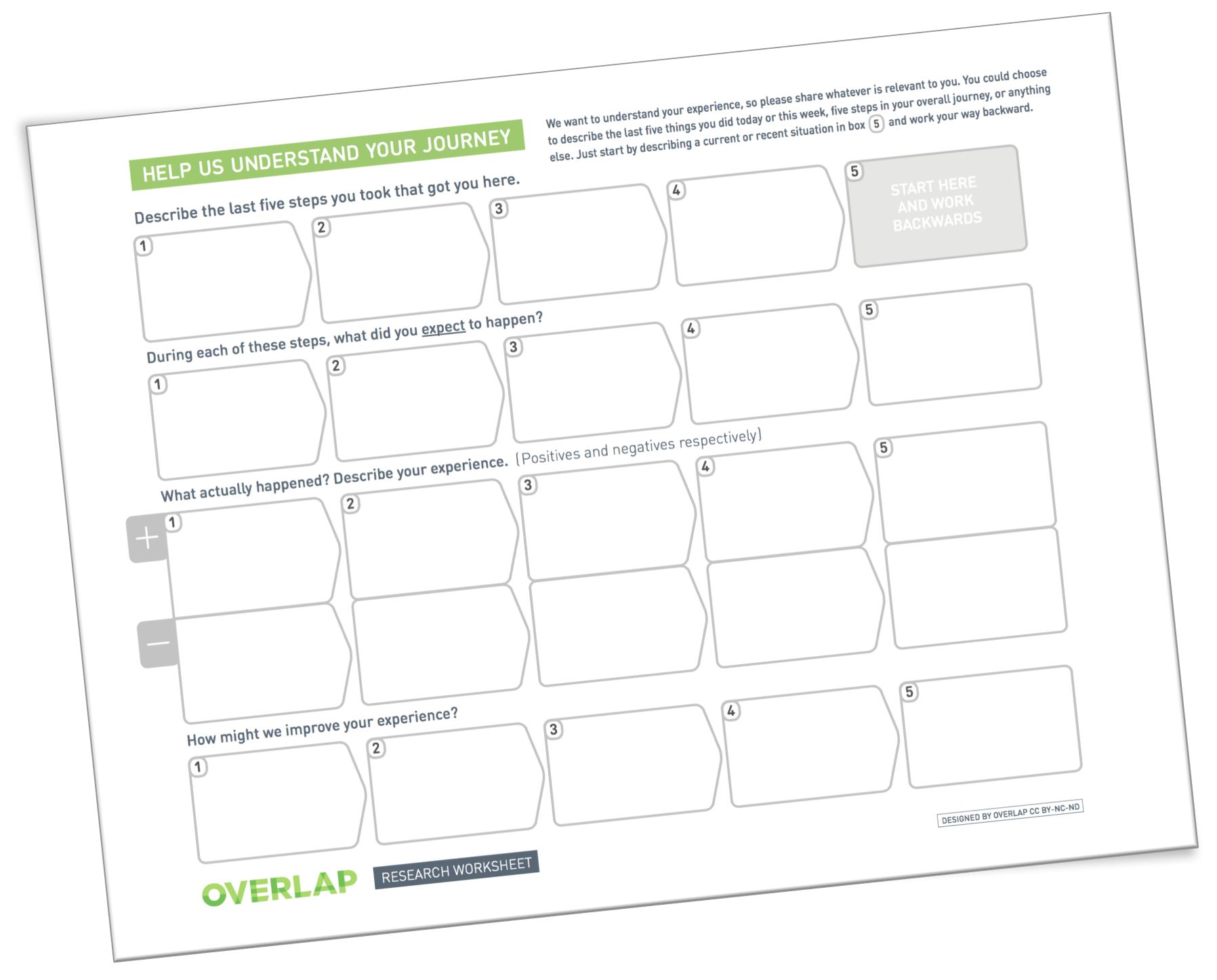
3. A Journey Map
Simply put, a journey map is a tool that helps us look at a person’s current experience so we can find ways to make it a better experience in the future.
When journey mapping, we ask people about:
The steps they took to get to where they are right now (often the waiting room, or having just finished their appointment)
What they expected or hoped would happen at each step
What actually happened, including what went well and what went poorly at each step
How their experience at each step could be improved
And follow along as you go through the instructions below:
You want to prompt people by asking them to describe the 3-5 things that have happened to them since they walked through our doors, or since they called you to receive your services, or whatever makes sense in your context.
Start with what they’re doing right now, and write that down in the grey box on the worksheet that says “start here”. Then follow up on their answer (“What happened before that?”, “And before that?”) and record those steps too. It’s okay if they work back and mention some things that happened before their arrival.
Listening to their experiences on the way to accessing your service is useful because:
1) perhaps we can help with an aspect of their journey
2) their journey has an impact on their needs when they arrive and
3) it may give important insight into the reason(s)—which may not be all medical—for their visit.
For each step:
Ask what they expected to happen.
What did they hope to do? Did they think it would be easy, or hard?
Ask about the positives and negatives.
What did they like? What didn’t they like? What went well and what was really challenging?
Ask about how they would improve the step.
What would they like to happen differently at that step, to make it better?
With these new tools in your pocket, you’ll be able to engage with your patients to better provide the kind of care they need, and the experience they desire.
Continue Learning:
75 Design Thinking Tools and Resources Explained
Harnessing the Power of Design Thinking in Addictions and Mental Health Care